
Thirteen patients experienced complete pain relief during the follow-up (mean 49.3 months).
#Aica vs pica syndrome plus
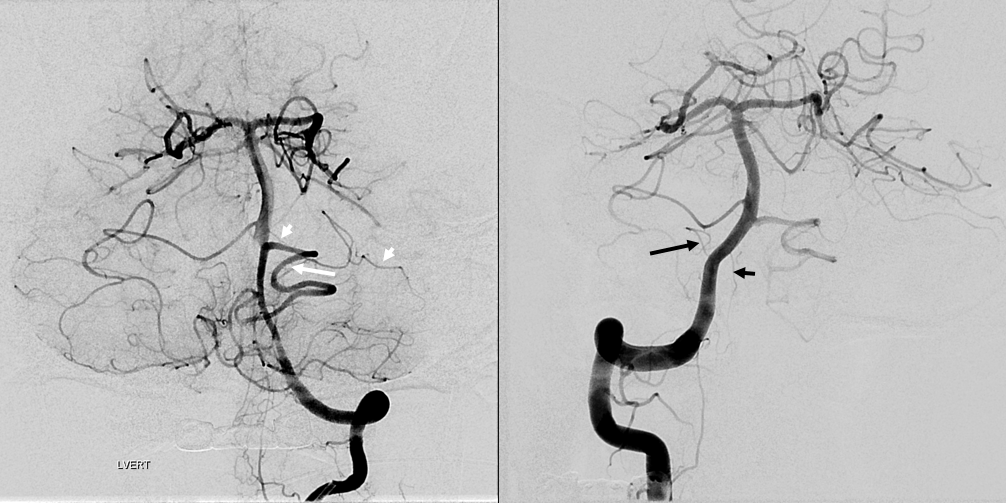
Seven patients underwent MVD plus glossopharyngeal nerve rhizotomy with or without partial vagus nerve rhizotomy. Seven patients underwent MVD of the offending vessel at the root entry zone (REZ) of the glossopharyngeal and vagus nerves. Swallowing was the most common trigger (85.7%) in these patients.
The pain area radiated to the trigeminal nerve distribution, including the anterior auricle (57.1%), temple (50%), cheek (28.6%), mandibular gingiva (42.9%), and anterior part of the tongue (14.3%). Information on pain recurrence and complications was collected.įourteen patients were recruited. The immediate and long-term outcomes were investigated to show the efficacy and safety of the treatment. All patients underwent surgical treatment. The aim of this study was to investigate the clinical characteristics and surgical outcome of microvascular decompression (MVD) with or without glossopharyngeal nerve and partial vagus nerve rhizotomy for treating glossopharyngeal neuralgia (GPN) patients with pain radiating to the area innervated by the trigeminal nerve.Ī retrospective review was performed to collect the clinical data from GPN patients who had pain in the area innervated by the glossopharyngeal and vagus nerves and radiating to the innervated area of the trigeminal nerve.

Nevertheless, with excellent surgical outcomes considered, MVD could still be a favorable treatment choice for combined HDS. Given that combined HDS tends to occur in elderly patients, surgeons should pay more attention to certain potential postoperative complications. Age and gender seemed to be independent risk factors for developing combined HDS. Studies regarding the prevalence of combined HDS are rarely reported the present ConclusionsĬombined HDS is an uncommon syndrome that usually occurs in females, and the most common types are combined TN-GPN and combined TN-HFS. In the present study, the clinical characteristics of combined HDS treated with MVD in our department were examined and discussed.Ĭombined HDS shows a tendency to occur in older female patients. 1 as a coexistent pathologic condition of the cranial nerve, such as TN, HFS, and GPN the syndrome occurs rarely and has rarely been investigated systematically. DiscussionĬombined HDS was first described in 1998 by Kobata et al. The demographic data, chronic comorbidities, and postoperative complications of combined HDS in Tables 3 and 4 were generally comparable with those of single HDS. Relevant demographic information, type of disease, vessels identified by the surgeon as compressing the root entry/exit zone (REZ), follow-up, and the surgical outcomes of patients with combined HDS are summarized in Table 1, Table 2, Table 3. 2)īrain tumor, arteriovenous malformation, other space-occupying lesions in the cerebellopontine area, and other forms of facial or oromandibular dystonic movements, focal seizures, tardive dyskinesia, history of Bell palsy, dystonia, blepharospasm, and metabolic diseases were excluded. Patients with combined onset of involuntary and asynchronous TN, HFS, and GPN, which may or may not occur simultaneously on 1 or both sides, were included. Section snippets Diagnostic Criteria and Data Sourceĭiagnostic criteria were as follows 2: 1) A total of 1450 cases of HDS underwent MVD in our department from January 2006 to September 2016, among which were 44 cases of combined HDS. In addition, the current study is the first to describe the incidence of several complications that occur after MVD with combined HDS.
#Aica vs pica syndrome series
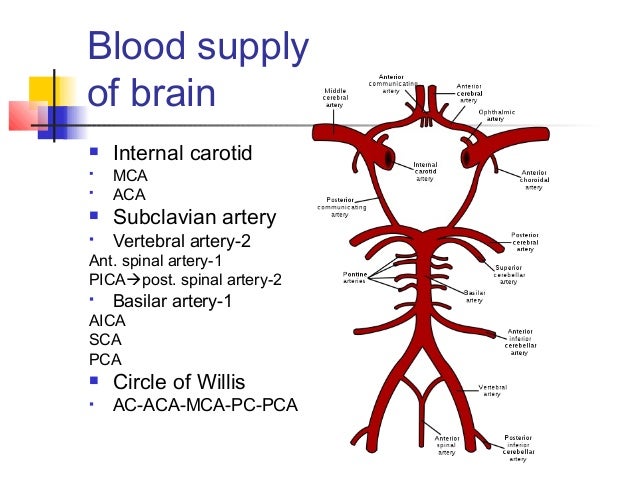
To our knowledge, isolated case reports or several small case series have thus far been studied,3, 4, 5, 6, 7 demographic characteristics, risk factors, and treatment effect after microvascular decompression (MVD) needs further study. Previous studies indicated that combined HDSs are extremely rare. These symptoms can sometimes occur synchronously or metachronously.1, 2 Combined HDS of cranial nerves is defined as the combination of HDSs that might or might not occur on 1 or both sides. Hyperactive dysfunction syndrome (HDS) is defined as symptoms arising from overactivity in cranial nerves, specifically, trigeminal neuralgia (TN), hemifacial spasm (HFS), and glossopharyngeal neuralgia (GPN), without an obvious explanatory structural lesion.


 0 kommentar(er)
0 kommentar(er)
